Colposcopy

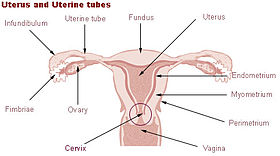
Colposcopy (Ancient Greek: κόλπος, romanized: kolpos, lit. 'hollow, womb, vagina' + skopos 'look at') is a medical diagnostic procedure to examine an illuminated, magnified view of the cervix as well as the vagina and vulva. Many pre-malignant lesions and malignant lesions in these areas have discernible characteristics that can be detected through the examination. It is done using a colposcope, which provides a magnified view of the areas, allowing the colposcopist to visually distinguish normal from abnormal appearing tissue and take directed biopsies for further pathological examination. The main goal of colposcopy is to prevent cervical cancer by detecting and treating precancerous lesions early. The procedure was developed by the German physician Hans Hinselmann, with help from Eduard Wirths. The development of colposcopy involved experimentation on Jewish inmates from Auschwitz. Colposcopy (Ancient Greek: κόλπος, romanized: kolpos, lit. 'hollow, womb, vagina' + skopos 'look at') is a medical diagnostic procedure to examine an illuminated, magnified view of the cervix as well as the vagina and vulva. Many pre-malignant lesions and malignant lesions in these areas have discernible characteristics that can be detected through the examination. It is done using a colposcope, which provides a magnified view of the areas, allowing the colposcopist to visually distinguish normal from abnormal appearing tissue and take directed biopsies for further pathological examination. The main goal of colposcopy is to prevent cervical cancer by detecting and treating precancerous lesions early. The procedure was developed by the German physician Hans Hinselmann, with help from Eduard Wirths. The development of colposcopy involved experimentation on Jewish inmates from Auschwitz. A specialized colposcope equipped with a camera is used in examining and collecting evidence for victims of rape and sexual assault. Most women undergo a colposcopic examination to further investigate a cytological abnormality on their Pap smears. Other indications for a patient to have a colposcopy include: Many physicians base their current evaluation and treatment decisions on the report 'Evidence-Based Consensus Recommendations for Colposcopy Practice for Cervical Cancer Prevention in the United States', developed by the American Society for Colposcopy and Cervical Pathology, most recently in 2017. Colposcopy is not generally performed for persons treated for cervical cancer if their pap tests show low-grade squamous intraepithelial lesion or less. Unless the person has a visible lesion, colposcopy for this population does not detect a recurrence of cancer. During the initial evaluation, a medical history is obtained, including gravidity (number of prior pregnancies), parity (number of prior deliveries), last menstrual period, contraception use, prior abnormal pap smear results, allergies, significant past medical history, other medications, prior cervical procedures, and smoking history. In some cases, a pregnancy test may be performed before the procedure. The procedure is fully described to the patient, questions are asked and answered, and the patient then signs a consent form. A colposcope is used to identify visible clues suggestive of abnormal tissue. It functions as a lighted binocular or monocular microscope to magnify the view of the cervix, vagina, and vulvar surface. Low magnification (2× to 6×) may be used to obtain a general impression of the surface architecture. 8x to 25x magnification are utilized to evaluate the vagina and cervix. High magnification together with green filter is often used to identify certain vascular patterns that may indicate the presence of more advanced pre-cancerous or cancerous lesions. Acetic acid solution and iodine solution (Lugol's or Schiller's) are applied to the surface to improve visualization of abnormal areas. Colposcopy is performed with the woman lying back, legs in stirrups, and buttocks at the lower edge of the table (a position known as the dorsal lithotomy position). A speculum is placed in the vagina after the vulva is examined for any suspicious lesions. 1% or 3% dilute acetic acid is applied to the cervix using cotton swabs. Areas of acetowhiteness correlate with higher nuclear density. The squamocolumar junction, or 'transformation zone', is a critical area on the cervix where many precancerous and cancerous lesions most often arise. The ability to see the transformation zone and the entire extent of any lesion visualized determines whether an adequate colposcopic examination is attainable.